Artikel von:
Carolyn Pierini
Quelle: http://www.cpmedical.net/articles/glutens-and-lectins-a-dangerous-dietary-duo
Healthcare practitioners and patients alike are familiar with the
increasing incidence and widening spectrum of gluten-related disorders.
Although celiac disease is the national icon of gluten sensitivity,
“atypical” presentations of the disease are rapidly becoming more
common, as is the concept of non-celiac gluten sensitivity.
Presently, gluten sensitivity or intolerance might best be defined as
a state of heightened immunological responsiveness in genetically
susceptible people. Gluten-related issues represent another star in a
constellation of growing public health concerns plaguing the U.S.
population.
Gluten Sensitivity on the Rise
On the surface, celiac disease offers an easy model of epigenetic
interplay—genetic predisposition (as HLA-DQ 2 or HLA-DQ 8) meets dietary
trigger as wheat gluten. In reality, gluten sensitivity is more complex
and better understood through the influence of diet and environment on
epigenetic factors responsible for amplifying or silencing multiple
genes.
Celiac disease represents one of at least 200 medical conditions,
involving nearly every organ of the body, which are now being linked to
gluten sensitivity.
1 In people with celiac disease, however,
the overall clinical picture is more severe and is accompanied by the
concurrence of tissue transglutaminase autoantibodies.
2
Transglutaminase enzymes are comprised of a family of eight enzymes
found throughout the body, including prostate, skin, lungs, testicles
and elsewhere. Because gluten triggers reactivity of this enzyme, all of
these tissues can be potentially affected.
Moreover, newly published research, sometimes inconsistent, is
unveiling the health effects of not only gluten, but other components of
wheat and non-wheat grains. The fact is, modern-day grain science is in
its infancy with regard to its impact on human health.
Given this, you, as clinicians, should understand why grain—and, in
particular, wheat-related gastrointestinal and related disorders—may be
increasing in your patient population.
Gluten Primer
The term “gluten” actually refers to a mixture of proteins found in
many grains including wheat, spelt, rye and barley. Lectins, often
included in this group, are technically not glutens, but are equally
important proteins found in several food groups, including grains.
Gluten literally means glue in Latin and is primarily composed of
“storage” proteins called glutelins (glutenins) and prolamines (named
for the high proline and glutamine content).
Gliadin is a type of prolamine and therefore a type of protein found
in gluten. Gliadins constitute the majority of protein found in wheat
and are thus far the most well-studied components of celiac disease.
3 Different types of glutens and lectins can be found in grain.
Many people are also sensitive to glutens and lectins found in other
non-wheat grain, particularly corn. Corn antibodies have been found in
patients with celiac disease, Crohn’s disease and ulcerative colitis.
4
Each seed or grain is composed of an outer bran layer, an endosperm
that houses 90 percent of these prolamines, and the germ nucleus, which
contains the developing plant embryo that will use the storage protein
as a nitrogen source during germination.
The Wheat Has Changed
The rise of wheat sensitivity in general may reflect the convergence
of many phenomena. The first point to consider is that modern commercial
wheat bears little resemblance to the wheat that sustained our
ancestors, which remained largely the same for 10,000 years... until
recent years.
In the past few decades, agricultural science has and continues to
use extensive hybridization, introgression and crossbreeding, making
“synthetic” wheat plants that are more resistant to drought and
pathogens. This has greatly increased dough properties but, more
importantly, yield and profit.
Seeds are equipped with anti-nutrients such as lectin, gluten,
phytates and enzymes to ensure protection from predation and resist
digestion long enough to be spread across the land through excretion.
Genetically selecting for anti-nutrients in an attempt to make the plant
more resistant and less costly to grow appears to have added an
increased threat to the gut immune system. New strains of wheat have
undergone innumerable, drastic transformations in their genetic code
yet, incredibly,
no human or animal safety studies were performed to gauge their suitability for human or animal consumption.5
The hybridization process increases the quantity of genes for gluten
proteins in modern wheat, including uniquely new gluten proteins not
found in the parent plants. This process is likely contributing to
gluten-related disease.
6-8 Perhaps it should not be
surprising that there is a naturally protective immune response to
ingesting more of something that is specifically designed to resist
digestion.
5 To quote one gluten researcher, “If we view
celiac disease not as an unhealthy response to a healthy food but a
healthy response to an unhealthy food, classical celiac symptoms like
diarrhea may make more sense.”
9
A Hidden Culprit
Also, beware of assuming that the primary causes of wheat intolerance
are directly attributable to gluten alone. In previous articles, we’ve
exposed wheat lectin for the serious problem it is. The wheat seed
embryo contains a tiny lectin called wheat germ agglutinin (WGA). It is
largely responsible for many pervasive ill-effects of wheat consumption.
WGA is inflammatory and capable of inflicting direct damage to the
majority of tissues in the body. It may help explain why degenerative
conditions are associated with heavy wheat-consuming populations, even
when wheat sensitivities appear uncommon.
By nature, lectins are resilient and resist degradation. Thus
soaking, sprouting, cooking and fermenting were historically implemented
in an effort to make grains such as wheat more digestible. Being a
powerful insecticide for the germinating seed, WGA has not escaped the
attention of biotech firms, which create genetically modified plants
with built-in WGA pest control.
As with gluten, selective breeding for particular proteins has
unfortunately led to proportionate increases in the WGA content of
modern-day wheat. The list of WGA-induced disruptions to health is
extensive and a reminder of how important the understanding of lectins
is.
Eating wheat delivers WGA to the gastrointestinal tract, where it can
cause mucosal injury and initiate inflammatory imbalance. WGA is small
enough to gain even greater access systemically through a leaky gut.
Anything that increases intestinal permeability, such as gluten or
NSAIDs, increases the likelihood of systemic inflammatory imbalance
created by WGA.
Although currently under-appreciated, WGA will eventually get its
share of the spotlight. In fact, some studies propose that WGA may
contribute in the pathogenesis of celiac disease. For example, one of
the hallmarks of celiac disease (crypt hyperplasia) appears to be due to
WGA’s ability to mimic the growth-promoting effects of epidermal growth
factor.
10 While serological antibody testing for WGA is
currently not performed, in one test study, antibodies to WGA were
demonstrated in the serum of celiac patients.
11
Our Love for Grains is Harming Us
A second point to consider is the sheer volume of ingested grain. In
2007, researchers in the United States, Italy and Great Britain
hypothesized that the incidence of celiac disease was on the rise
worldwide because wheat had become so prevalent in the Western diet that
humans are actually overdosing on it.
It is true. Modern-day wheat is found in nearly everything we
consume: cereal and flour-containing items, food and drink additives,
grain-derived alcoholic beverages and even medications and cosmetics.
This is exemplified by a 2005 study, which revealed that an
unprecedented epidemic of symptomatic celiac disease in Sweden was at
least half explained by an increase in infant exposure to comparatively
large amounts of gluten as a result of national dietary recommendations
and infant food content.
12
Foundationally, microbial interactions in the gastrointestinal tract
provide the cues for the development of regulated pro- and
anti-inflammatory signals that promotes immunological tolerance.
13
Doctors report that it is not uncommon to see patients with a
conglomeration of gastrointestinal symptoms due to exposure to gluten
and lectin of wheat and other grains.
The gliadin protein of gluten in all forms of wheat is capable of
increasing intestinal permeability by triggering the release of zonulin,
a protein that disassembles tight junctions between intestinal cells.
14 Small intestine bacterial overgrowth (SIBO),
15 gastroesophageal reflux disease
16 and intestinal
Candidiasis17-18 are all associated with gluten intolerance. Additionally, a 2009 research review in the
Journal of Gastroenterology
suggests that patients with irritable bowel syndrome (IBS) be
genetically tested for gluten sensitivity, as symptom resolution was
observed with wheat elimination.
The health consequences of consuming wheat extend beyond the immune
system, making diagnosis complicated for physicians. For example, wheat
exorphins exhibit addictive effects on the brain and nervous system, and
wheat’s high glucose-insulin effects contribute to cardiovascular
disorders, diabesity, hormone imbalance and acne.
19-20 Complete removal of wheat or other grains is often necessary to deconstruct the clinical picture.
Gluten-Free Foods—Not Always the Perfect Answer
It is helpful to caution patients using “gluten-free” alternatives to
replace the wheat proteins. In addition to being a source of
insulin-provoking carbohydrate, alternatives such as sorghum, millet,
corn, barley, oats or other grains and starches contain their own
gluten/lectin proteins, which may cause problems in gluten-sensitive
people.
21-23
The majority of the population is not aware that their present health
and weight problems have anything to do with environmental factors, and
certainly not the iconic “healthy” whole grains. After all, Americans
are encouraged by government and private groups, advertising and
elements of the healthcare community to eat them at every sitting.
There is a looming public perception that if you don’t have celiac
disease, you don’t have a wheat problem. However, the belief that modern
grain is a healthy food is just not sufficiently supported by facts.
Grain education to change deeply held convictions about food will be a
formidable challenge, but a worthy one.
Resources
1. http://theglutensyndrome.net/primer.pdf.
2. Sapone A, et al. BMC Medicine. 2011;9:23.
3. www.glutenfreesociety.org.
4. Davidson IW, et al. Clin Exp Immunol. 1979 Jan;35(1):147-8.
5. Davis W. Wheat Belly. New York: Rodale. 2011 pg 14-30.
6. Song X, et al. Theor Appl Genet. 2009;118(2):213-25.
7. Gao X, et al. Planta. 2010;23(2):245-50.
8. Van den Broeck HC, et al. Theor Appl Genet. 2010;121(8):1527-39.
9. http://www.greenmedinfo.com/page/dark-side-wheat-new-perspectives-celiac-disease-wheat-intolerance-sayer-ji.
10. http://www.glutenfreesociety.org/gluten-free-society-blog/wheat-germ-agglutinin-wga/.
11. Sollid LM, et al. Clin. Exp. Immunol. 1986;63(1):95-100.
12. Ivarsson A, et al. Best Pract Res Clin Gastroenterol. 2005;19(3):425-40.
13. Vitetta L, et al. Inflammopharmacology. 2012 Mar 18.[Epub ahead of print].
14. Drago S, et al. Scand J Gastroenterol. 2006;41:408-19.
15. Rubio-Tapia A, et al. J Clin Gastroenterol. 2009;43(2):157-61.
16. Levine A, et al. Scand J Gastroenterol.2009;44(12):1424-8.
17. Nieuwenhuizen WF, et al. Lancet. 2003;361(9375):2152-4.
18. Staab JF, et al. Science. 1999;283(5407):1535-8.
19. Rudman SM, et al. J Invest Dermatol. 1997;109(6):770-7.
20. Cordain L, et al. Arch Dermatol. 2002;138:1584-90.
21. Kristjansson G, et al. Gut. 2005;54:769-74.
22. Sandhu JS, et al. Gut. 1983;24:825-30.
23. Troncone R, et al. J Pediatr Gastroenterol Nutr. 1987;6(3):346-50.
Quelle: http://www.cpmedical.net/articles/glutens-and-lectins-a-dangerous-dietary-duo
Mauerbergstraße 110
76534 Baden-Baden
Tel.: 07223 / 8004699
Mobil: 0177 / 4977232
Mail: info@aktiv-training.de
Fax: 07223 / 8005271
Mobility-Walking: http://mobility-walking.blogspot.com
Personal Fitness: www.personal-fitness-4u.de
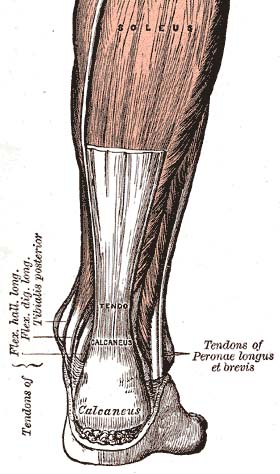 Not
much literature exists regarding the treatment of myotendinous Achilles
ruptures. The authors conducted this study in order to retrospectively
examine clinical outcomes from uniform nonsurgical treatment of these
injuries. Between November 2005 and May 2011, 30 patients presented with
an acute, complete myotendinous Achilles rupture. The location of the
Achilles injury was confirmed on magnetic resonance imaging (MRI) for
all patients. All patients were treated nonsurgically, with a system
including 3 weeks of non-weight-bearing and then 3 weeks of progressive
to full weight-bearing in an Achilles boot. Physical therapy was
provided for 4 to 6 weeks after this period of immobilization. 21 males
and 9 females participated. The patients had a mean age of 40.8 years
(range, 24-54). Patients were followed an average of 40.5 months (range,
23-81). They achieved full healing of the Achilles myotendinous
junction clinically in all 30 patients . All patients experienced
improved function and less pain at their latest follow-up. Mean Foot and
Ankle Ability Measure-Sports (FAAM-Sports) increased from 20.2% at the
time of initial presentation to 95.2% at the latest follow-up (P <
.05). Mean Visual Analog Scores (VAS) of pain decreased from 8.2 at the
time of initial presentation to 1.3 at latest follow-up (P < .01). In
all, 23 (76.7%), 6 (20%), and 1 (3.3%) patients rated their
satisfaction as excellent, good, an
Not
much literature exists regarding the treatment of myotendinous Achilles
ruptures. The authors conducted this study in order to retrospectively
examine clinical outcomes from uniform nonsurgical treatment of these
injuries. Between November 2005 and May 2011, 30 patients presented with
an acute, complete myotendinous Achilles rupture. The location of the
Achilles injury was confirmed on magnetic resonance imaging (MRI) for
all patients. All patients were treated nonsurgically, with a system
including 3 weeks of non-weight-bearing and then 3 weeks of progressive
to full weight-bearing in an Achilles boot. Physical therapy was
provided for 4 to 6 weeks after this period of immobilization. 21 males
and 9 females participated. The patients had a mean age of 40.8 years
(range, 24-54). Patients were followed an average of 40.5 months (range,
23-81). They achieved full healing of the Achilles myotendinous
junction clinically in all 30 patients . All patients experienced
improved function and less pain at their latest follow-up. Mean Foot and
Ankle Ability Measure-Sports (FAAM-Sports) increased from 20.2% at the
time of initial presentation to 95.2% at the latest follow-up (P <
.05). Mean Visual Analog Scores (VAS) of pain decreased from 8.2 at the
time of initial presentation to 1.3 at latest follow-up (P < .01). In
all, 23 (76.7%), 6 (20%), and 1 (3.3%) patients rated their
satisfaction as excellent, good, an